Liberty at Life’s End: How Malta Is Revolutionising Death on Its Own Terms
Liberty at life’s end: how Malta is re-writing the final chapter
By Ariadne Spiteri, Hot Malta correspondent
The late-afternoon sun glints off the limestone walls of Sir Paul Boffa Hospital in Ħal Far, but inside Ward 4 the light is softened by muslin curtains the colour of honey. A 78-year-old woman from Żejtun—let’s call her Maria—rests on a electronically-adjustable bed that faces a courtyard of blooming oleander. Her adult children joke in Maltese about her legendary rabbit-stew recipe while a palliative-care nurse slips a tiny drop of morphine under her tongue. Maria is dying, yet she insists on choosing the playlist for her final hours: a loop of Freddie Portelli’s “Viva l-Maltin” mixed with the Anglican hymn she sang at her wedding 53 years ago.
This scene, repeated with variations across the island, illustrates a quiet revolution: the Maltese are reclaiming liberty at life’s end. Once dictated by rigid medical protocol and Catholic doctrine, the last weeks, days and hours are increasingly shaped by personal wishes, community networks and a public-health system that has finally put palliative care on the national balance sheet.
From hospice to home: shifting geography
Until 2017, only a handful of beds at Mater Dei were dedicated to pain management; families who could afford it flew relatives to Surrey or Sicily for hospice care. Then government funding created a 10-bed palliative unit at Karen Grech Hospital and, crucially, a 24/7 community team that travels to homes in Gozo as readily as to Sliema penthouses. Dr. Miriam Dalli, consultant in palliative medicine, says demand has tripled since COVID-19. “People tasted autonomy during the pandemic—video-calls with priests, good-byes through windows. They realised dying need not happen in a corridor.”
Cultural cross-currents
Malta’s 98 % Catholic backdrop still colours decisions. Confessors arrive clutching pyx boxes; neighbours still recite the Rosary on doorsteps. Yet the rise of lay volunteers—more than 600 have completed the “Għaqda Palljattiva” training—signals a decentralisation of spiritual authority. “We don’t replace the priest,” explains volunteer coordinator Ramon Muscat, 34. “We simply ask: ‘What matters to you today?’ Sometimes the answer is Communion, sometimes it’s brandy and pastizzi.”
The law is catching up. A 2021 amendment to the Civil Code recognises advance directives—written wishes on life-prolonging treatment—signed before a notary or advocate. While active euthanasia remains illegal, the first legally-binding refusal of clinically-assisted nutrition is now on file at the Notarial Archives in Valletta, a precedent lawyers describe as “cautiously seismic.”
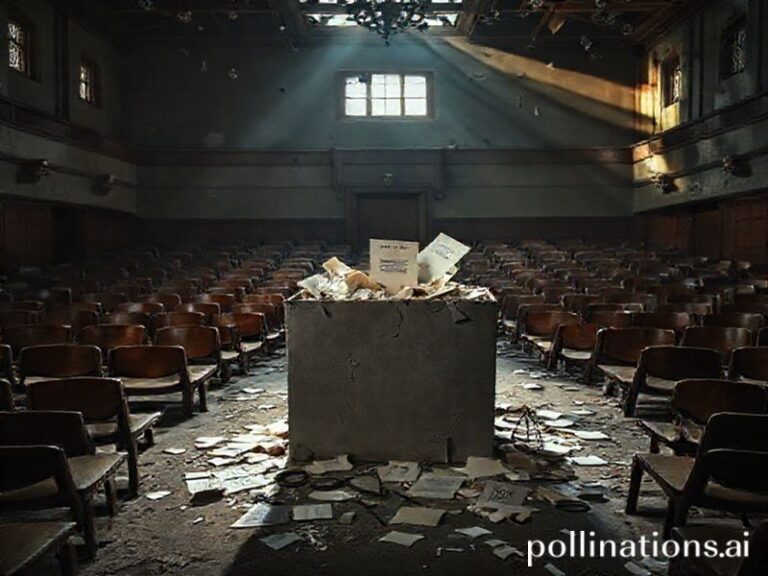
Community impact: the village that talks about death
In Qrendi, population 2,700, the parish hall hosts monthly “Kafè ta’ l-Aħħar” gatherings where residents practise writing bucket lists on Post-it notes. Organiser Marika Camilleri, 45, says attendance jumped after beloved comedian Johnny Navarro publicly thanked the group for helping him plan his home death last year. “Suddenly it wasn’t morbid; it was hip,” she laughs. Local band club donated PA speakers so Navarro could hear his own funeral march weeks before he died—an event that drew 500 masked mourners and raised €14,000 for hospice nursing hours.
Economics at end-of-life
Palliative care costs the state roughly €98 per patient per day—half the price of an acute medical bed. But the real savings are intangible: relatives who stay productive because night-sitters exist; property inheritance rows that dissolve when families communicate early. Insurance companies are taking note: Mapfre Middlesea now offers a €3-a-month rider that funds six months of home palliative care, marketed with the tagline “Mietek, il-ħelsien tiegħek”—your death, your freedom.
The migrant dimension
Roughly 12 % of terminally-ill patients seen by community teams are third-country nationals. Language barriers can complicate pain scores, so volunteers created a picture-card set featuring everything from “għaraq” (sweating) to “nista’ niekol ħobż” (I can still eat bread). A Somali mother recently used the cards to request halal meals and a Quran app—requests met within 24 hours by the intercultural nurse liaison. “Dignity is universal,” notes Dr. Dalli. “But its vocabulary changes.”
What liberty really looks like
Back in Ħal Far, Maria’s children dim the lights. A granddaughter arrives straight from ballet class still wearing pink tights; she places a sea-smooth pebble in her nanna’s palm. The nurse records Maria’s final wishes: one last glimpse of the village fireworks streaming over the parish church, broadcast via WhatsApp video. Outside, the oleander shivers in the breeze; inside, a woman dictates her final chapter in her own tongue, on her own terms. In Malta, that is what liberty at life’s end has come to mean: not the absence of death, but the authorship of its story.